After a cesarean (C-section) delivery, your body sets in motion a healing process at multiple depths: skin, subcutaneous fat, fascia, abdominal muscles (which are separated or moved aside during surgery, not cut), and the uterine wall.
The incision is typically (but not always) made in the lower abdomen. Understanding how scars form helps you know if, when and how massage may help.

C-Section Scars
A C-section, or cesarean section, is a major surgery performed to deliver a baby through an incision in the abdomen and uterus.
As with any surgical procedure, the body’s natural healing process leads to the formation of a scar at the incision site.
C section scars can look and feel different from person to person, depending on factors like:
-the type of incision
-your body’s healing response and
-how you care for the wound after surgery (this being one of the most important steps!)
Understanding the types of c section scars, how they heal, and what you can do to minimize scarring can help you feel more confident and in control during your recovery.

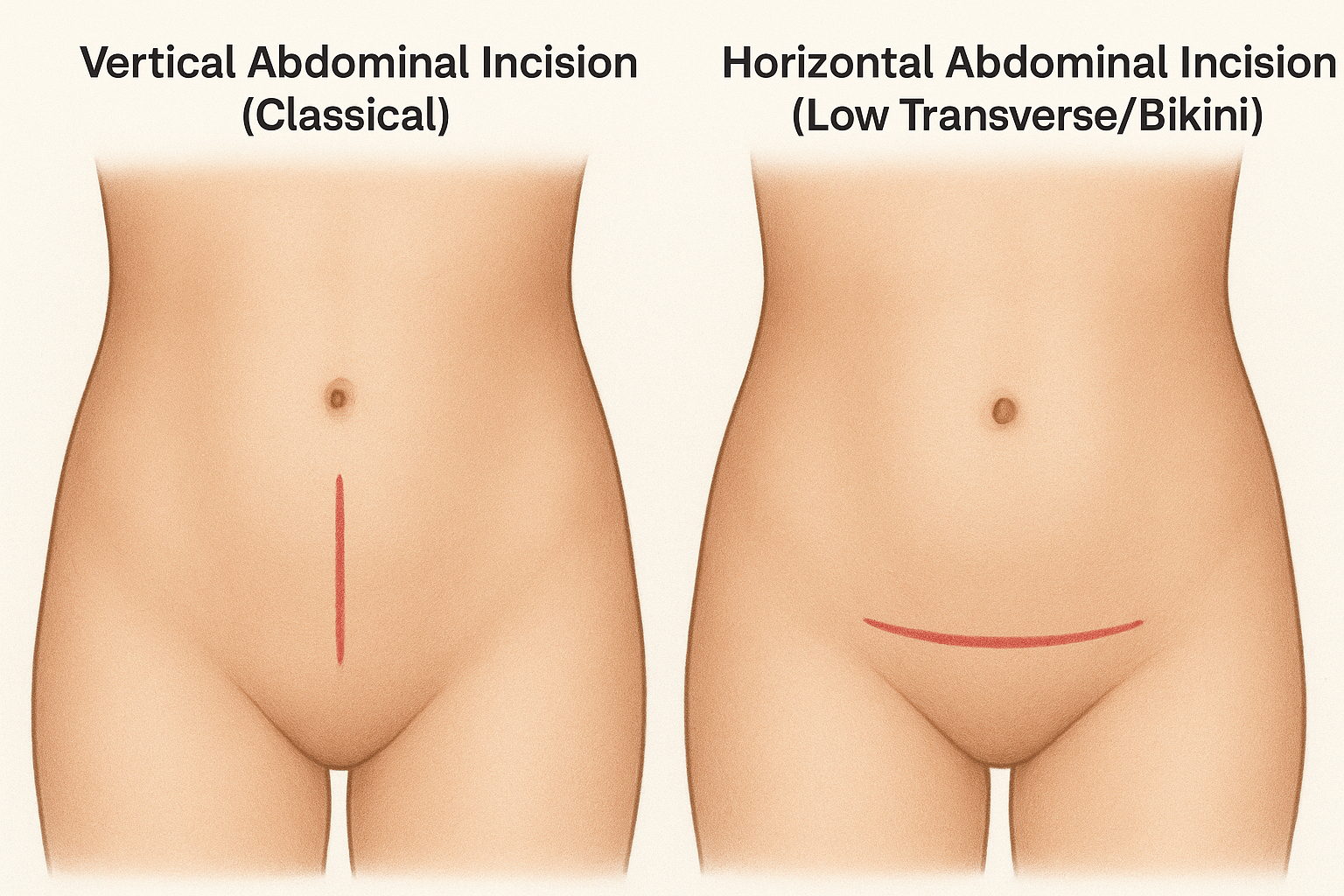
C-Section: Incision Types
During a C-section, your surgeon will make two incisions: one through the skin and abdominal wall, and another through the uterus.
The abdominal incision can be either a vertical incision (running up and down the midline) or a horizontal incision, often called a bikini cut, which runs just above the pubic hairline.
Vertical incisions, sometimes referred to as classical incisions, are typically reserved for emergency situations or when the baby or placenta is in an unusual position, as they allow for quicker access.
However, most planned C-sections use a horizontal (or low transverse incision) because it tends to heal with a less noticeable scar and carries a lower risk of complications.
The uterine incision itself is usually also a low transverse incision, matching the abdominal incision for optimal healing and future pregnancy safety.
The type of incision you have can influence the appearance and healing of your section scar, as well as your overall recovery experience.
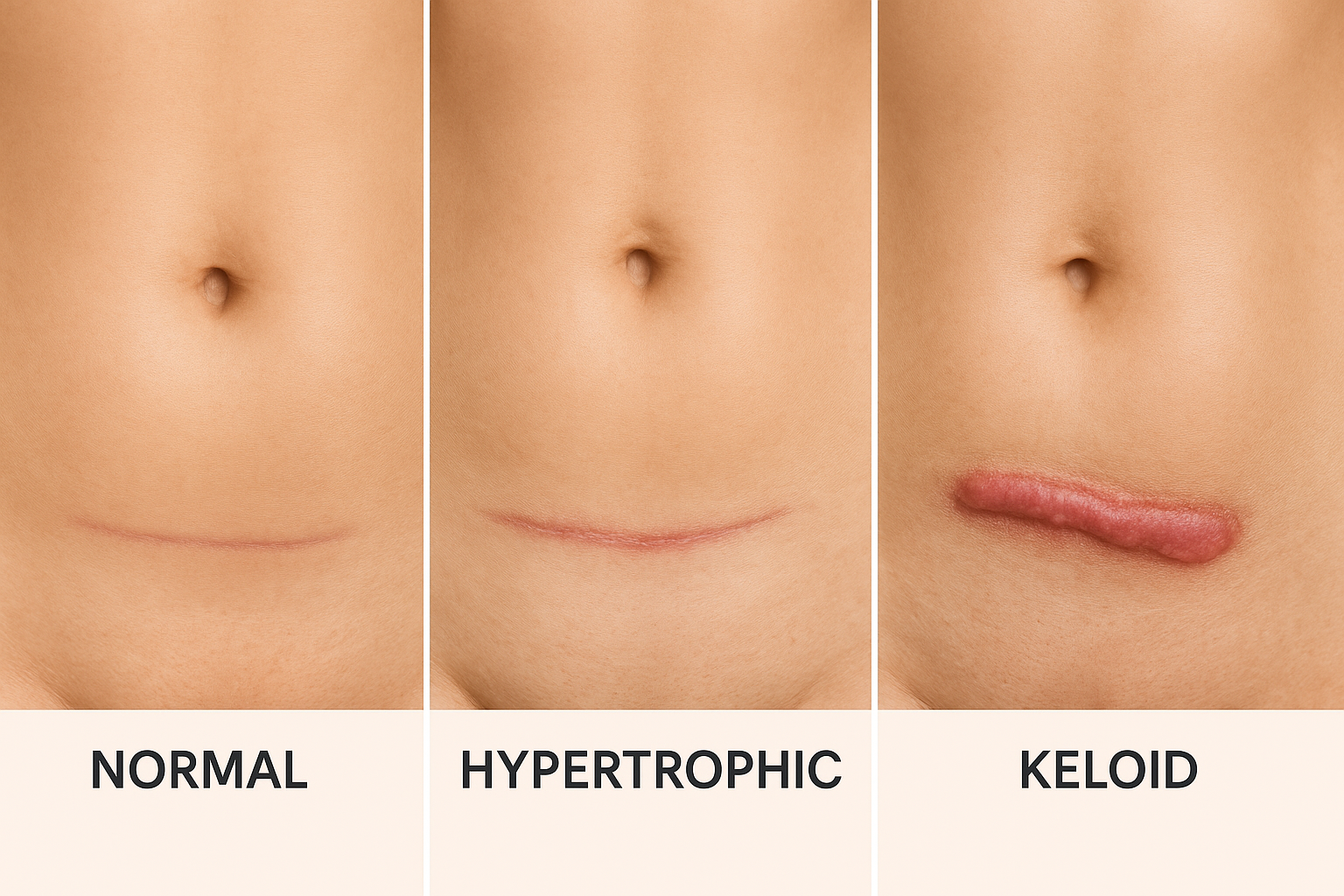
Types of Scars
Not all C-section scars look or feel the same. The way your scar heals depends on your body’s unique response to surgery, as well as the type of incision and how you care for the wound.
Some people develop hypertrophic scars, which are thick, raised scars that stay within the boundaries of the original incision line.
Others may experience keloid scars, which are raised, firm, and extend beyond the original scar tissue, sometimes forming noticeable lumps around the incision site.
Genetics, skin type, aftercare and certain medical conditions can make you more prone to developing hypertrophic or keloid scars.
The Stages of Scar Healing
Scars don’t heal overnight—they move through three natural stages.
The timings below are typical for surgical cuts like a C-section:
1) Haemostasis & inflammation —
first few hours to about 3–5 days
What your body’s doing:
blood clots to stop bleeding; your immune system clears away germs and debris. This “clean-up” creates some swelling and redness.
What you might notice:
the area feels tender, warm, and puffy.
2) Proliferative —
around days 5–14 (sometimes up to 3–4 weeks)
What your body’s doing:
it lays down new collagen (the early, softer kind called Type III), grows tiny new blood vessels, and pulls the wound edges together.
What you might notice:
a raised, pink-to-red line that can be itchy at times.
3) Remodelling / maturation —
weeks to months (can continue for 1–2 years)
What your body’s doing:
the early collagen is reorganised and upgraded (from Type III to stronger Type I). Over time the scar becomes softer, flatter, and paler.
What you might notice:
gradual flattening, less redness, and the skin feels more flexible again.
Two important notes!
- Deeper layers (like fascia and muscle) take longer to settle than the skin you can see. It’s normal for full scar “maturity” to take up to two years after surgery.
- Because this slow reshaping goes on for months, gentle scar massage/mobilisation can still be helpful well beyond the early weeks.
Be patient—the scar is more delicate at first, and pushing too hard too soon can set healing back.

Why Scars Sometimes Cause Issues
Even when the skin “looks healed”,
beneath the surface things may not glide freely.

These are some of the reasons why this may be the case:
- Adhesions: The scar may stick to tissues underneath (fascia, muscle) and reduce movement or cause pulling sensations.
Scar tissue can also form adhesions that affect internal tissues and organs such as the colon, ovaries, bladder, and uterus! - Stiffness / reduced mobility: The scar (and tissues around it) may feel tight or “frozen”
- Pain or discomfort / hypersensitivity: Some women report pain locally (especially on pressure), a sore midsection, or sharp tugs with movement.
- Altered sensation / numbness: Nerves in the area might be traumatized during surgery.
- Aesthetic concern: Raised or hypertrophic scars, pigment changes, widening scars. C-section scars may also appear darker than the surrounding skin, especially in individuals with darker skin tones.
Because of these issues, clinicians often recommend gentle mobilization or massage of the scar once it’s safe.
The Role and Benefits of Scar Massage or Mobilisation
Scar massage is essentially a manual technique to gently mobilise the scar tissue and surrounding tissues so that layers don’t adhere excessively, collagen fibres align more functionally, and soft tissue mobility is improved.
Physical therapy can also play a key role in scar healing and recovery after a C-section, supporting tissue mobilization and addressing complications.
What does the evidence say?
- A review of 25 studies (1,515 participants) found that scar massage may help reduce pain, increase movement, and improve scar characteristics—but the studies were variable in their methods, making concrete conclusions difficult.
- A proof-of-concept study in women with C-section scars (with 32 participants - so a very small study!) showed that just two sessions of standardised mobilization improved scar stiffness, elasticity, and pressure pain thresholds (small to moderate effect sizes) over a short term.
- A broader systematic review of manual scar therapy (massage plus complementary methods) showed benefit in reducing pain, improving pliability, reducing pigmentation/itching, and improving cosmetic appearance of postoperative scars.
- A case series (2 participants only!) of chronic C-section scar pain used fascial release techniques (stretching scar until release) and reported large improvements in pressure tolerance and pain scores over 4 weeks.

In short: The evidence is limited but supportive.
Scar massage is a low-risk, low-cost, non-invasive addition that many women find helpful for symptom relief, scar flexibility, and comfort.
As part of a comprehensive c section recovery plan, scar massage can support both physical healing and scar appearance. It should always complement—not replace—proper wound care and guidance from your medical team.

Why is massage helpful (in simpler terms)?
- Helps to soften stiff scar tissue and prevent binding between tissue layers
- Promotes better alignment of collagen fibres (so the scar is less rigid)
- Enhances local circulation and lymph drainage (bringing nutrients, removing waste)
- Helps reduce itching and hypersensitivity by gentle desensitization
- Improves the mobility of skin and deeper tissues, potentially reducing pulling, tugging sensations
- May reduce discomfort (pain) in some women
When and How to Perform C-section Scar Massage Safely
Getting the timing and technique right is very important—too early or too forceful and you risk damaging healing tissue.
It is essential to wait until the incision has had time to heal completely before beginning scar massage.

When Can You Start?
This is one of the most asked questions.
Only begin scar mobilisation once the wound heals and is fully healed: there should be no scabs, open areas or discharge.
Most NHS providers suggest 6 - 8 weeks post-C-section as a safe window for beginning, as by then the superficial skin has healed.
Some sources state you might begin gentle external or indirect mobilisation slightly earlier, but not directly on the scar until the superficial skin has healed.
If ever unsure, always check with your obstetrician, midwife, GP, or physiotherapist.
Because remodelling of the scar continues for up to 1–2 years, starting later may still bring some benefit, but earlier is better for preventing tight scars.

Preparation: What To Do Before Massage
- Clean hands and clean skin:
Wash your hands and gently wash the area beforehand. Some guides recommend washing off moisturizer or oil before massaging to avoid occlusion. - Use a lubricant:
A non-perfumed cream, emollient (E45) or massage oil will reduce friction but still allow you to “grab” the tissue enough to mobilise. - Position comfortably:
Lying or semi-reclined posture, knees bent, relaxed abdomen, use pillows as needed. - Warmth/softening:
Some sources advise using a warm compress or taking a warm shower before to relax tissue and improve blood flow. - Go gradual:
Start with light pressure and progressively increase as comfort improves. Never use pressure that causes sharp pain.

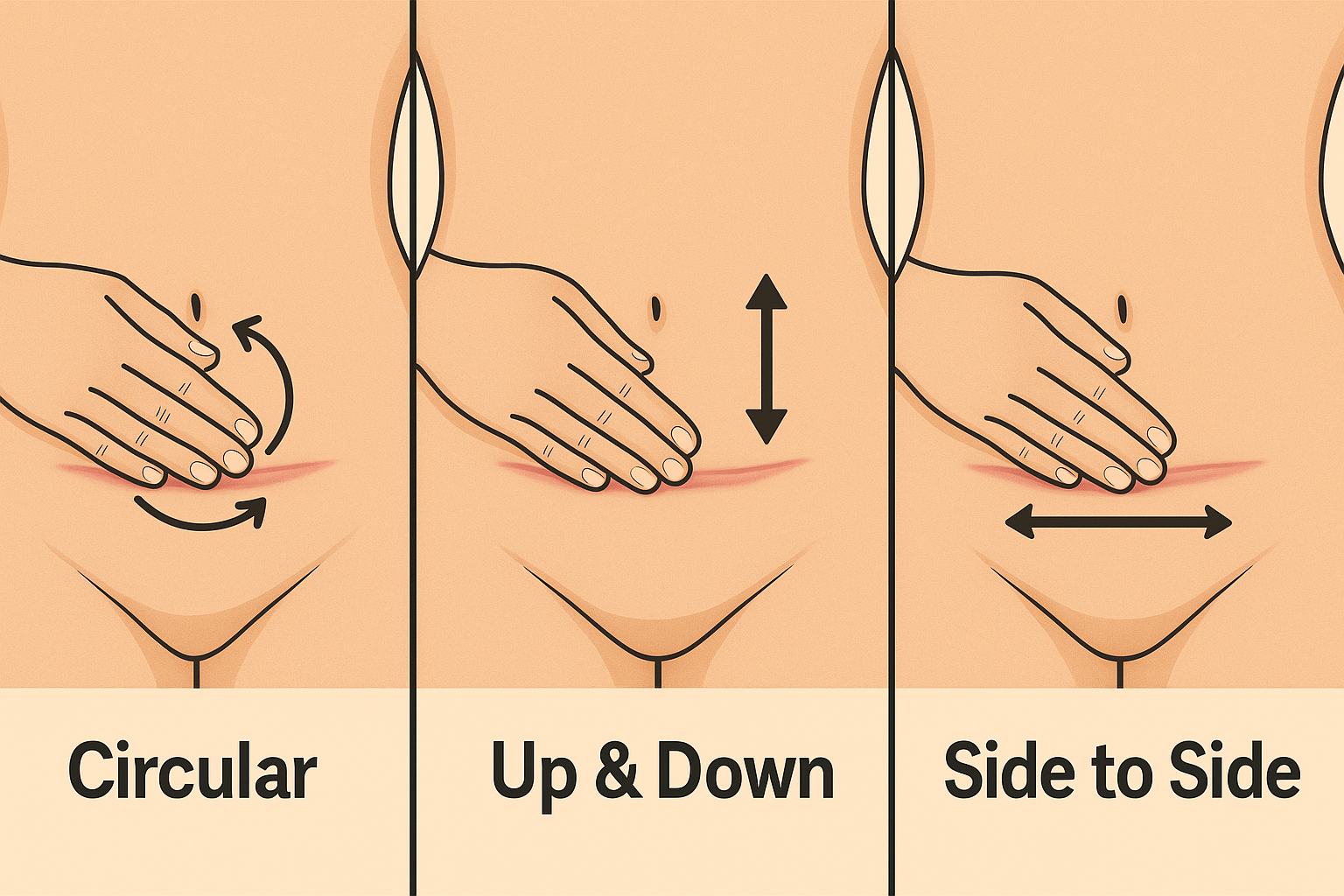
Technique: step-by-step method
- Start around the scar
- Begin by massaging the skin and tissues just above and below the scar (rather than over it) to “wake up” surrounding tissue.
- Gently move the skin in small circles, or shift it side to side and up/down.
- Circular motion
Using the pads of 2-3 fingers (or thumb) make small circular movements over and around the scar, both clockwise and anticlockwise, 5–10 times. - Vertical / longitudinal strokes
Along the length of the scar, run up-and-down strokes (i.e. gently lift and move the scar tissue lengthwise). - Horizontal / transverse strokes
Gently slide the scar sideways (left-right) across the width, moving from side to side. - “Stretch-hold” / sustained stretching
If you find a spot where the scar “sticks,” hold gentle pressure in the direction of least mobility for 5–10 seconds until the tissue “gives.” Many guides call this a “release.” - Scar rolling / pinching (ADVANCED stage)
Once the scar is less tender, carefully pinch up skin and subcutaneous tissue and “roll” it between fingers (thumb + finger), moving along the length of the scar, side to side and up/down. Do this gently and only when tissue is ready. - Deep mobilisation (under supervision)
As your comfort and mobility improve, you may introduce deeper mobilization (into fascia and muscle layers) as long as there is no pain or irritation. Many physiotherapists or women's health therapists can guide this.
Frequency and Duration
- Cambridge University Hospitals suggests at least 2–3 times a day, 5 minutes each time
- Frequency can be reduced once scar movement improves.
- Be consistent: scar tissues respond better to regular gentle stimulation than irregular heavy pressure!

When To Stop Or Modify Massage
Stop and seek professional advice if:
- The scar becomes redder, swollen, warmer, bleeds or discharges
- Pain is worsening significantly or is sharp
- A rash or blister appears
- There is any reopening or tearing of skin
Always move gently, listen to your body, and gradually increase intensity only when no irritation occurs.

Tips and Cautions
- Avoid massaging too early (before skin fully heals) to prevent damage or reopening
- Use enough pressure to feel movement, but never push into sharp pain
- Scar massage should feel like a stretch, not a bruise
- You can combine massage with silicone gel / sheets — some evidence supports its use
- Protect scar from sun (use SPF 30+ or cover it) while it’s healing
- Maintaining a healthy diet can support optimal scar healing and recovery
- If you experience psychological discomfort (e.g. trauma from past surgery) when touching the scar, start gently (e.g. over clothes) or seek help from a women’s health physiotherapist or counsellor.
Putting it all together: sample schedule
(weeks to months)
Here’s a rough timeline you can adapt based on your healing:
Period | Focus / goals | Massage approach |
|---|---|---|
Weeks 0–6 | Skin wound healing, risk of reopening | No direct massage. Light touching around scar, breathing, gentle mobility (per guidance). |
Weeks 6–8 | Begin gentle mobilisation once skin is healed | Start with superficial massage around scar (circular, gentle strokes). 1–2 times daily lightly. |
Months 2–6 | Increase intensity, add deeper layers | Introduce vertical, horizontal strokes, stretch-holds, rolling, deeper mobilisation as comfort allows—2–3 times/day up to ~10 min. |
6 months – 1 year | Maintenance, deeper remodelling | Continue massage 2–3 times per week; address stubborn tight areas; may reduce frequency but remain attentive. |
Beyond 1 year | Scar is nearing maturity | Benefit may taper but targeted massage for tight spots may still offer improvement. |
Note: Your individual healing may be faster or slower—adjust accordingly and always follow medical advice!

What To Expect (Realistically)
What you can reasonably expect:
- Gradual softening and flattening of scar
- Improved mobility of skin and underlying tissues
- Reduced itch, discomfort, and pulling sensations
- Some improvement in cosmetic appearance over time
Limitations and caveats:
- Scar massage is not a “magic fix”: results are incremental, subtle
- Evidence for scar massage is positive but imperfect: many studies have methodological limitations.
- Some scars (e.g. hypertrophic or keloid) may respond differently and may need medical attention.
- If a scar is badly formed, wide, or functionally problematic, you may need other interventions (e.g. revision surgery, steroid injections or laser therapy under medical supervision)
- You may not “erase” the scar—but you can often improve how it feels and looks
Frequently Asked Questions (FAQs)

Is it safe to massage before 6 weeks?
Generally, no—massaging too early (while tissue is still fragile) risks tearing, irritation, or infection. Wait until the scar is fully closed, scabs have fallen off, and there is no discharge. Always confirm with your healthcare provider.
Can I massage if my scar is more than a year old?
Yes, albeit with more modest expectations. The scar continues remodelling for up to 1–2 years, so you may still gain some increased mobility or softening of tight spots. However, the “window” for major structural change diminishes.
How long before I see results?
Some women feel early improvements, such as less discomfort, more pliability, and even less pain, within weeks, but deeper changes (less stiffness, flattening) often take months of consistent work. Clinical studies have shown measurable changes even after just two sessions, but meaningful remodeling takes longer.
Does massage reduce scar appearance (colour, height)?
Massage can help with scar pliability and texture, and may somewhat influence cosmetic appearance, but it is not a guaranteed cosmetic correction. However, a hypertrophic or keloid scar may respond differently to massage and often requires additional treatments from dermatologists or plastic surgeons.
If massage hurts, should I stop?
Yes—pain is a signal. If massage produces sharp pain, swelling, redness, bleeding, or discomfort that lingers, stop and seek medical input. Gentle discomfort (“stretching feeling”) is expected, but not severe pain.
Can a partner or therapist do the massage?
Yes—once you're comfortable, a trusted partner (who is shown the technique above) or a trained therapist (e.g. women’s health physiotherapist) can help. They may reach deeper or catch things you might miss. Always ensure they are gentle and follow safe technique guidelines.
Should I combine massage with other scar therapies?
Yes, in some cases combining treatments can be more effective. Evidence supports manual therapy + complementary methods (such as silicone sheets, taping, micro-needling) over single methods alone.



